Experts urge nutrition integrated into childhood cancer treatment

HEALTH specialists have called for nutrition to be formally integrated into childhood cancer treatment protocols, warning that failure to address malnutrition undermines therapy outcomes and survival rates.
The call follows findings from a study conducted by paediatric health experts at Muhimbili National Hospital, presented during the 30th anniversary celebrations of the Ocean Road Cancer Institute in Dar es Salaam late last week.
Researchers concluded that structured nutritional support significantly improves children’s dietary status, reduces complications linked to malnutrition and enhances the effectiveness of chemotherapy and other cancer therapies.
According to the study team, many children undergoing cancer treatment face appetite loss, nausea and difficulty eating — side effects that frequently result in weight loss and weakened immunity. Without targeted nutritional intervention, these conditions can delay treatment cycles, reduce tolerance to medication and increase the risk of infections.
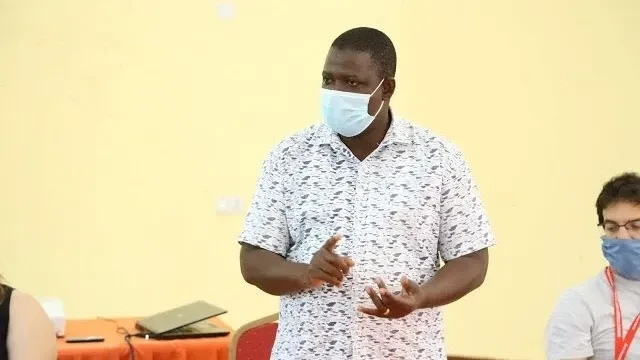
Ruchius Philbert, assistant principal investigator of the childhood cancer nutrition project and a public health specialist, said nutrition must be treated as a core component of therapy rather than an optional add-on.
“Nutrition is not just a supplement; it is part of the treatment,” he said. “Proper nutrition strengthens the body’s ability to fight disease. Children need not only medication but also the right diet to maximise treatment outcomes.”
He explained that children experiencing feeding challenges require tailored dietary strategies, including specialised meal plans and clinical nutrition support, to prevent deterioration during treatment.
Leading the study, Dr Hadija Mwamtemi, a paediatric oncology specialist, urged health authorities to embed nutrition as a mandatory element in childhood cancer care protocols nationwide.
She noted that while medical advances have improved cancer survival rates, gaps in supportive care, particularly nutrition — continue to compromise outcomes.
“Integrating nutrition into standard treatment guidelines will improve survival rates, reduce complications and enhance the quality of life for young patients,” she said.
The findings have sparked broader discussion among clinicians and policymakers about strengthening multidisciplinary cancer care, including collaboration between oncologists, dietitians and nursing teams.
Childhood cancer cases in Tanzania have been rising steadily, with specialists attributing the increase partly to improved diagnosis and referral systems. However, experts caution that survival rates in low- and middle-income countries remain significantly lower than in high-income nations, often due to late diagnosis and limited supportive care.
Health professionals say formalising nutritional services within oncology units could represent a cost-effective intervention with measurable impact.
Top Headlines
© 2026 IPPMEDIA.COM. ALL RIGHTS RESERVED