Deputy minister highlights gaps in Marriage Act’s clause on epilepsy

DEPUTY minister of Health Dr Florence Samizi has acknowledged that Tanzania’s Marriage Act contains provisions that contribute to the stigma faced by people living with epilepsy.
Section 39(a)(ii) of the Act allows couples to petition for divorce if one partner is diagnosed with epilepsy—a clause Dr Samizi described as outdated and discriminatory.
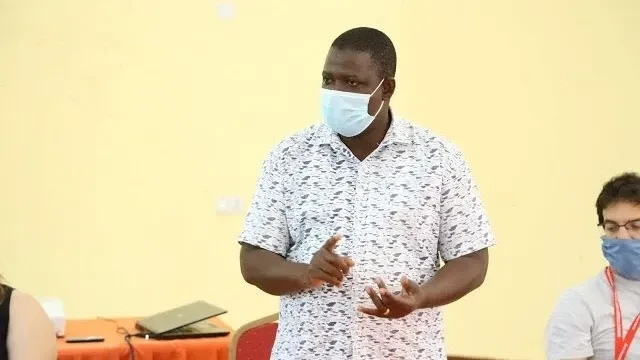
Speaking yesterday during the World Epilepsy Day commemoration in Dar es Salaam, Dr Samizi urged lawmakers to review the law, noting that it unfairly singles out epilepsy while ignoring other neurological conditions such as stroke or memory loss.
“This is a law the ministry treats with great seriousness and one that must be reviewed. If someone suffers a stroke or begins to experience memory loss, these are also neurological conditions,” Dr Samizi said. “Why, then, is separation suggested only in cases of epilepsy? Parliament and Members of Parliament are responsible for law-making, and this matter requires urgent examination.”
The Deputy Minister also cautioned service providers—particularly in public institutions such as health facilities and schools at all levels—against discriminating against patients and students with epilepsy. She highlighted that stigma remains one of the key barriers to effective care and social inclusion.
“It is our responsibility to improve public understanding of epilepsy. This year’s theme reminds us of the need for collective action,” she said, stressing the importance of communities supporting individuals who experience seizures rather than ostracising them.
Dr Samizi added that the ministry has made significant strides in improving access to anti-epileptic medicines. Availability has increased from about five per cent in 2020 to between 50 and 80 per cent across various categories, including phenobarbital. She also emphasised the need for clear clinical guidelines, adequate budget allocations, and strengthened service delivery to improve epilepsy care nationwide.
“In both health institutions and the education sector, we must confront stigma in all its forms: self-stigma, institutional stigma, and societal stigma,” Dr Samizi said.
Prof William Matuja, chairperson of the Tanzania Epilepsy Association (TEA), said stigma remains pervasive, affecting communities, institutions, and patients themselves. He noted that about 70 per cent of people with epilepsy seek hospital care late due to fear of discrimination.
“Awareness of epilepsy in the community is still low. An estimated one million people in Tanzania are living with the condition, which in many areas continues to be associated with myths and misconceptions,” Prof Matuja said.
He added that people with epilepsy have historically faced isolation and marginalisation. “During my postgraduate research in Mahenge, I found many patients living in extremely challenging conditions. In over 30 years working in this field, stigma has remained the greatest challenge.”
Prof Matuja identified three main forms of stigma: self-stigma, societal stigma, and institutional stigma, citing the Marriage Act and limited government budget allocations as contributing factors.
He called on the government to collaborate closely with stakeholders to reduce stigma and improve care. “To address gaps in epilepsy diagnosis and treatment, we need more trained specialists, a national programme, lessons from international experience, and sustained public education on the condition,” he said.
Prof Matuja also proposed the establishment of a national coordination committee to oversee initiatives aimed at addressing epilepsy-related challenges.
Top Headlines
© 2026 IPPMEDIA.COM. ALL RIGHTS RESERVED