Sustaining mpox response in Africa as efforts starting to bearing fruit

WHILE mpox remains a global threat—underscored by WHO’s declaration on 22 November 2024 that it continues to constitute a Public Health Emergency of International Concern (PHEIC)—in Africa, we are beginning to see positive signs that response efforts are paying off.
Since August 2024, when mpox was declared a Public Health Emergency of International Concern, globally, the situation has become more complex. And as the disease can spread through international travel, it still needs a coordinated international response.
This is not to say, however, that the situation in Africa is the same as just over 100 days ago.
The mpox situation in Africa is nuanced. Many countries in the region have strengthened disease surveillance, case detection (including at points of entry during travel), infection prevention (including through vaccination), and the provision of care and support for affected individuals. All these efforts have contributed to curbing the spread of the virus.
For example, since October 2024, the Republic of Congo, Gabon, Guinea, and South Africa have reported no active mpox outbreaks for at least six consecutive weeks and entered the “control phase” (the control phase kicks in when no new cases have been reported in the last 42 days). And as of 25 November, Ghana, Zambia and Zimbabwe have also entered the control phase.
Sixteen of the 19 mpox-affected countries in the region have now achieved testing rates above 80 percent However, the Democratic Republic of the Congo continues to dominate case counts, accounting for close to 80 percent of all lab-confirmed cases in the region since the start of the year.
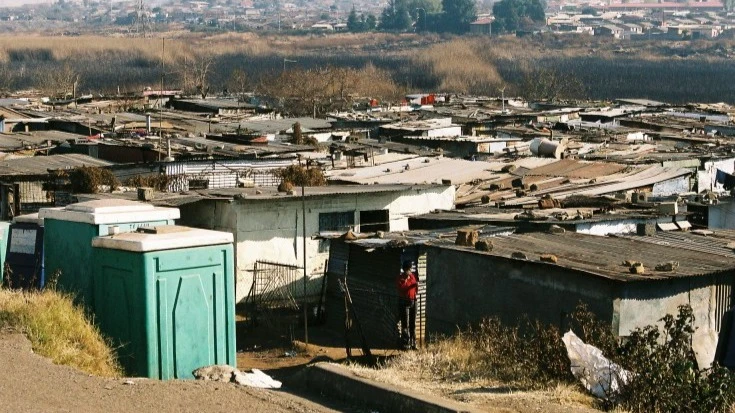
Mpox has spread to over 80 percent of health zones (424 out of 519) across the Democratic Republic of the Congo, with South Kivu, Tshuapa, and Sankuru currently bearing the highest burden. The country faces significant challenges, including limited diagnostic capacity and logistical constraints. For example, only 37 percent of collected samples were tested in the three weeks spanning late October to early November 2024, leaving some provinces underrepresented in surveillance data and impacting the response.
We must continue our efforts in all key areas of outbreak response and strengthen our efforts where needed.
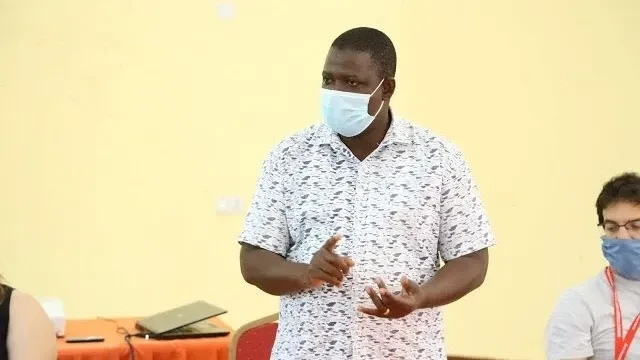
Across the region, WHO, Africa Centres for Disease Control and Prevention and partners have provided a wide range of technical and material support to governments to help them prepare for and respond to mpox outbreaks. More than 2000 health workers have been trained in the key aspects of outbreak response; diagnostic capacity has been vastly expanded with the delivery of 42 000 PCR (or polymerase chain reaction) tests in October alone; contact tracing and treatment have been ramped up; and large-scale risk communication and community engagement activities are being actively supported to inform populations on how to stay safe.
In addition, WHO is providing technical support to countries to develop targeted vaccine deployment plans to maximize the impact of a limited number of doses. It has made it easier for countries to procure vaccines by adding the MVA-BN vaccine to its prequalification list; triggering the emergency use listing process for LC-16 and ACAM2000 vaccines; and establishing an Access and Allocation Mechanism (AAM) to facilitate better access to vaccines, treatments and tests where they are most needed.
Mpox vaccination campaigns are being rolled out in the Democratic Republic of the Congo, Nigeria and Rwanda and vaccination plans are underway in other countries.
In November, AAM has allocated close to 900 000 mpox vaccine doses to nine African countries hardest hit by mpox surge. They include the Central African Republic, Cote d’Ivoire, the Democratic Republic of the Congo, Kenya, Liberia, Nigeria, Rwanda, South Africa and Uganda.
During a recent visit to a treatment centre in Kinshasa, the Democratic Republic of the Congo’s capital, I saw first-hand the efforts and the challenges faced by health workers who are continuing to work tirelessly under challenging conditions.
As of 27 November 2024, 12 countries still had active transmission of the virus. Eight of them—the Democratic Republic of the Congo, Burundi, the Central African Republic, Nigeria, Côte d’Ivoire, Liberia, Uganda and Kenya—have outbreaks of high concern. Of these, Burundi, the Democratic Republic of the Congo and Uganda collectively account for more than 96 percent of all lab-confirmed mpox cases in the region, continue to need urgent and sustained interventions.
The IHR Emergency Committee at its second meeting on the upsurge of mpox on 22 November 2024 noted the progress towards controlling the spread of mpox but advised that the event continues to meet the criteria of a public health emergency of international concern, and that there is a need for sustained a cohesive response across countries, including stronger national commitments.
Whilst we acknowledge gains and celebrate successes to date, no doubt, we need to do more to keep populations safe from mpox, in Africa and elsewhere.
Global and regional solidarity is key. More resources and support, especially for the communities and countries that are bearing the brunt of the mpox outbreak in Africa, is key.
Only then, can we consolidate gains and address remaining challenges, be that around surveillance or access to mpox vaccines.
As of 27 November 2024, more than 14 669 lab-confirmed cases with 55 deaths had been reported in the African region in this year. Case reports of the highly virulent clade 1b strain in the United Kingdom, Sweden, Germany, the United States of America, Thailand and India highlight the urgent need to tackle this outbreak at its epicentre to prevent further global spread.
Mpox is a viral illness caused by the monkeypox virus, a species of the genus Orthopoxvirus. Common symptoms of mpox are a skin rash or mucosal lesions which can last 2–4 weeks accompanied by fever, headache, muscle aches, back pain, low energy and swollen lymph nodes. In severe cases, the disease can be deadly.
Top Headlines
© 2025 IPPMEDIA.COM. ALL RIGHTS RESERVED