Quiet Revolution? How NGOs steered Tanzania’s Universal Health Coverage Evolution

IN recent years, talk of Universal Health Coverage (UHC) has dominated headlines in Tanzania, often triggered by public concerns over health insurance— and at times, milestones of hope such as the enactment of the landmark Universal Health Insurance (UHI). However, there was a time when UHC seemed like a distant dream for the country, yet at that time, a quiet revolution was brewing – one spearheaded by Non-Governmental Organizations (NGOs), working in tandem with government authorities right from the grassroots.
Over a decade and a half ago, Dr Heri Marwa, by then fresh from graduating with a Master’s in Health Policy, Finance and Management at Muhimbili University of Health and Allied Sciences (MUHAS), witnessed firsthand the milestones of the UHC agenda; the humble beginnings, the tough decisions and what it took for the country to come up with the national version of the Improved Community Health Insurance (ICHF)—a scheme that had sparked his curiosity at university.
Dr Marwa’s zeal was particularly timely as Tanzania was just four years away from drafting its Healthcare Financing Strategy (2015-2026), although the document has remained unsigned over the years.
Today, as Dr Marwa recounts the untold story of UHC in Tanzania, he has already transitioned to Country Director of PharmAccess Tanzania, a Dutch non-profit organization which he joined as manager right after graduating. By the time he joined the organization, PharmAccess—at international level—was laying the groundwork for a long-held mission to address health system challenges in Africa through improved health insurance access and quality healthcare.
“When I joined PharmAccess that’s when we went to launch KNCU Health Plan,” he said in an interview recently, recalling a story that dates as far back as 13 years ago, when the Kilimanjaro Natives Cooperative Union (KNCU) Health Plan was beginning to sprout.
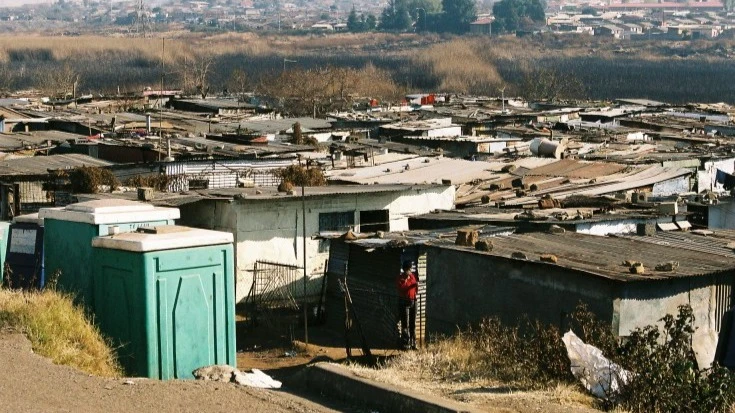
The KNCU Health Plan had been designed to provide affordable and quality healthcare services to coffee farmers and their families who are affiliated with KNCU. It was established in response to the challenges faced by coffee farmers in accessing adequate healthcare. Many of the farmers in rural areas (just like other farmers in the country) had limited access to healthcare facilities and often could not afford the costs of medical treatment. As of 2013, the plan had enrolled over 15,000 members.
“But before I even joined the organization, a lot of effort on UHC had been ongoing. UHC has been in the DNA of PharmAccess,’’ he said, taking us back to the early days when his organization came into being, and what this came to mean for the UHC efforts in Tanzania today.
While PharmAccess is now prominently associated with UHC efforts, its roots lie in addressing HIV/AIDS crisis in Africa. Founded in 2001 by Dr Joep Lange, a physician and researcher working at the University Hospital in Amsterdam, the organization emerged from a stark realization. He was one of the world's top HIV/Aids researchers and prominent pioneer of antiretroviral therapy who died aged 59 in the crash of the Malaysia Airlines flight MH17 in eastern Ukraine in 2014.
During his work, he had witnessed the readily available Antiretroviral Therapy (ART) for HIV patients in Amsterdam, and was deeply troubled by the lack of access of the same in Africa.
In one of his visits to Uganda in 1992, he saw children born with HIV and their families struggling with helplessness. Unlike the well-resourced and informed gay communities accessing ART in Amsterdam, much of Africa faced a different reality. Driven by this disparity, Dr Lange returned to Amsterdam and advocated with the government for support to Africa. He then went on to convince large multinational companies.
Dr Marwa recall: "Lange made a compelling argument. He highlighted the financial implications of losing trained employees to HIV-related illnesses. It was a strategic move that demonstrated the potential of private-public partnerships in healthcare."
At the time, there was a prevailing belief that complex healthcare interventions like HIV treatment were not feasible in Africa. Critics argued that African populations lacked the necessary knowledge and infrastructure. Dr Lange defied these assumptions.
That’s how the first HIV clinic in Delta State, Nigeria, was opened then followed by another in Namibia. These successful pilot programmes provided crucial evidence that effective HIV treatment was indeed possible in Africa, challenging the prevailing skepticism.This also paved the way for major initiatives like the Global Fund and the US President's Emergency Plan for AIDS Relief (PEPFAR).
However, access to HIV treatment was just one piece of the puzzle. With more Western support, access to HIV treatment improved significantly. Yet, one big question arose: What if patients with HIV succumbed to malaria due to a lack of affordable treatment for other illnesses?” This led PharmAccess to tackle the broader challenges of healthcare financing and quality of care. This would ensure that patients who pre-paid for care actually received the services they needed, fostering trust in the system.
In 2006, PharmAccess received significant funding from the Dutch government. This enabled them to open offices in four African countries, including Tanzania, with the goal of innovating better access to quality healthcare. In Tanzania, the first health insurance project kicked off in 2009, focusing on women microfinance recipients.
Faced with a choice between medical care for their children and repaying loans, the women were particularly vulnerable. PharmAccess successfully partnered with PRIDE, a microfinance provider and Strategis Insurance, to offer health insurance bundled with loans, ensuring their wellbeing and financial stability. The KNCU Health plan came after these initiatives.
“When we started, there were already Community Health Fund (CHF) schemes in every district in the country,’’ he said, adding: “That was the original CHF.” But as CHF gained momentum, challenges arose.
How iCHF was born
People began to opt for the KNCU Health Plan which had started earlier, even if they weren't members of the KNCU and the premium was twice that of CHF, leading to concerns among regional authorities.
“Despite facing resistance, we persisted, recognizing the need to improve the existing community health insurance model,” he said.
“Our focus was on ensuring that everyone had access to health insurance. The KNCU Health Plan resistance by the region authority came with the opportunity to collaborate with the existing CHF. We knew that by improving the CHF, we would have a sustainable scheme, which could reach a wider population".
Through a collaborative process, PharmAccess worked with district authorities to identify and address weaknesses in CHF such as lack of clear reimbursement model, lack of proper pooling policy where in some districts it was done at facility level and other facilities at district level, both resulting into limited risk sharing among enrollees. The administration of the scheme also required a lot of improvements.
The reforms led to the establishment of the Improved CHF or (iCHF).
“So, with iCHF we decided to add a social insurance feature in the community scheme. For example, we said we should have someone who manages it at regional level, not at district level. NHIF was the best option,’’ he said.
PharmAccess advocated for a regional approach to allow for a larger risk pool and increase management efficiency. A clear benefits package was established to ensure transparency and avoid confusion among beneficiaries. A system of capitation payments was introduced to provide service providers with predictable income based on the number of patients enrolled. This incentivized quality care and reduced uncertainty. But also a referral system was implemented to ensure patients could access higher levels of care when needed, including faith-based health facilities.
Although the changes came with an increase of contributions from 10,000 to 30,000, people welcomed it because they were assured of receiving the services they paid for when enrolling into the scheme.
Partnering with NHIF
A key aspect of iCHF's success was its collaboration with the National Health Insurance Fund (NHIF) which played a key role in regional pooling mechanisms to ensure a more equitable distribution of funds across different areas. But also NHIF acted as the regional administrator, handling administrative tasks and ensuring smooth operations. NHIF also played a role in enrolling members into the iCHF programme, expanding its reach and payment of providers.
There was a noticeable improvement in healthcare services. PharmAccess's success in Kilimanjaro and Manyara attracted attention from other regions, paving the way for the national rollout of iCHF.
“We started very successfully. We went on to 14 percent enrolment by the first year. And then people were like, ‘you know you are succeeding because Kilimanjaro is relatively richer than other regions’, so we decided also to expand to Manyara,’’ he said, explaining however, that PharmAccess was not alone in the efforts.
Other NGOs and international organizations were also experimenting with different models and approaches. In Dodoma Region, the Swiss Programme HPSS developed its own model, while GIZ implemented a different model in Lindi and Mtwara regions.
While these organizations had varying approaches, they shared a common goal of strengthening CHF and improving healthcare access. “Their collective efforts contributed to a rich landscape of innovation and experimentation and this helped the government to scale up the UHC efforts,” he said.
The success of iCHF in Kilimanjaro and Manyara regions demonstrated its scalability and adaptability. PharmAccess expanded the programme to Manyara in 2016, achieving even greater success.
In 2019, the government called upon all partners supporting CHF to discuss improvement of the community health funds. . PharmAccess's regional based model iCHF stood out due to its innovative approach and demonstrated success. The government recognized the value of the model and adopted it as the foundation for the national UHC initiative. The other models also had their contribution in shaping the national model.
“We were the only ones with a regional model, and realistic and yet reasonable premium,’’ Dr Marwa said. Despite its successes, iCHF faced challenges during the national rollout.
One key issue was the decision to remove the defined benefits package. This made it difficult for facilities owned by faith-based organizations to participate, limiting the reach of iCHF. Additionally, changes to the payment model and referral system had unintended consequences, affecting enrolment and service quality.
As the country moves towards UHI, Dr Marwa emphasized the importance of innovation and adaptation in achieving UHC. Tanzania's unique context, with a large informal sector, requires tailored solutions. By challenging traditional approaches and embracing new ideas, NGOs and government agencies can overcome obstacles and find effective ways to deliver healthcare to all.
Can Tanzania attain UHC by 2030?
While Tanzania has made significant strides, challenges remain.
Dr Marwa believes that it is possible to achieve UHC by 2030. He pointed to the support from the President Samia Suluhu Hassan who has shown political will and the existence of necessary laws and regulations. Despite the good signs, he also acknowledged that implementation has been slow.
"We have to put beneficiaries at the centre of our initiatives, " he said. Despite the challenges, Dr Marwa remains optimistic. He cited examples of other countries like Cambodia that have achieved UHC in a relatively short period.
"It is possible but we need to work on innovations to address the existing challenges," he said.
The author is a science journalist who focuses on public health, medicine and research communication. He can be reached via at [email protected]
Top Headlines
© 2024 IPPMEDIA.COM. ALL RIGHTS RESERVED