Kagera to reduce maternal, child mortality with new clinic cards

IN a ground-breaking move to enhance provision of healthcare services, Kagera Region has unveiled new clinic cards for expectant mothers and children, a move aimed to significantly bolster government efforts to reduce maternal and child mortality rates.
The initiative, part of a broader government strategy, underscores the region’s commitment to improve public health outcomes and ensure every mother and child receive the care they deserve.
Sr MaryGoreth Rusingiza, is the Kagera Regional Reproductive and Child Health Coordinator (RRCHCO), she told The Guardian that between January and June 2024, there were 25 maternal deaths and 109 perinatal deaths compared to 2023 records where there were 56 maternal deaths were and 227 infant deaths.
“The number of deaths is going down; we need to do more on stillborn babies (macerated stillbirths) which are still high. This kind of deaths occur before pregnant mothers go for labour; it is caused by various diseases especially when the mother had never received proper neonatal care at a hospital or health center,” explained Sr MaryGoreth.
On June 25, 2024, the Kagera Regional Administrative Secretary, Steven Ndaki, received 63,473 clinic cards, comprising of 31,411 cards for child growth records and 31,411 for pregnancy health records. The official handover took place at the Regional Commissioner’s office.
Ndaki expressed gratitude to the government for addressing the shortage of clinic cards, saying the move would greatly help in reducing maternal and child mortality rates. He urged healthcare providers to use them as intended to improve maternal and child health services.
Kagera Regional Medical Officer, Dr Samwel Laiser said the newly launched clinic cards would be distributed across all eight districts. Laiser challenged health care providers to ensure ethical distribution and proper use of the cards.
“The government through the Ministry of Health has provides these cards for purposes of monitoring maternal and child health in our region. We are going to offer them for free, hence the need for the community to cooperate with healthcare providers to ensure they are used as intended,” said the official.
Health Minister Ummy Mwalimu took a decisive step to ban the sale of clinic cards during a launch event in Dodoma recently. She stated: “This move underscores the Tanzanian government’s unwavering commitment to maternal and child health as a top priority, aiming to meet the Sustainable Development Goals (SDGs).
Mwalimu emphasized improvements of the cards to meet current needs, with an estimated annual requirement of two million pregnant women and new-borns.
Director of Mother and Child Services at the Ministry of Health, Dr Ahmad Makuwani, said a total of 1,200,000 books would be distributed across the country. Of the number, 600,000 cards are for expectant mothers and 600,000 for children.
"The goal is to ensure that important information of the mother during pregnancy is properly taken to the extent that service providers can put their recommendations on what should be done to ensure both, the pregnant mother and the child are safe,” said Dr Makuwani.
Deputy Secretary General in the Ministry of Health, Dr Grace Magembe, highlighted that producing enough clinic cards aims to eliminate a significant barrier for mothers. "Mothers avoided clinics because they were being charged for these cards.
The government has now printed enough cards and will continue to print them annually to alleviate this burden," Dr. Magembe explained.
The Kagera region's proactive approach and the government's firm stance against commercialization of the clinic cards highlight their dedication to enhance healthcare outcomes for mothers and children.
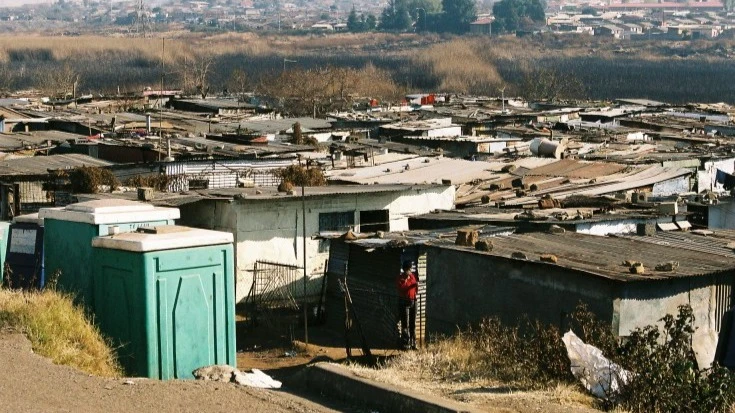
Home birth fines and health cards are products of a major global push for increased numbers of institutional deliveries in low and middle-income countries over the last two decades.
The maternal mortality ratio (MMR) and the proportion of women giving birth under skilled care have become a major measurements of maternal health success and failure. Maternal mortality, however, is difficult to count in countries without reliable civic registration systems.
Skilled birth attendance has therefore become an important proxy indicator for MMR and is often seen as the main indicator of maternal health progress in low-resource settings today. Skilled birth attendance, however, is also often difficult to measure.
Despite insufficient evidence, it is often assumed that an increase in the number of institutional deliveries leads to a reduction in maternal mortality.
Efforts to combat maternal mortality, aimed at increasing facility births, have become a push for numbers. This push has shifted the focus away from discussions of skilled birth attendance and the quality of care, onto the indicator of institutional deliveries itself.
It has also led to the proliferation of new, localized policies aimed at increasing facility births. A growing body of literature documents sanctions against women who give birth at home in Malawi, Zambia, Burkina Faso, and Tanzania.
Top Headlines
© 2025 IPPMEDIA.COM. ALL RIGHTS RESERVED