Expand choices for women, prevent new HIV infections in Africa

IN Uganda, women and girls are more affected by HIV. Out of 1.4 million people living with the disease, 860 000 are women and girls.
According to UNAIDS, every week, 4,000 adolescent girls and young women aged 15–24 years became infected with HIV globally in 2023, with 3,100 of these infections occurring in sub-Saharan Africa.
In 2023, in sub-Saharan Africa, women and girls accounted for 62 percent of all new HIV infections.
As part of the efforts to prevent new infections and death among the adolescents and women, Uganda adopted oral PrEP in 2017, or pre-exposure prophylaxis. PrEP, or pre-exposure prophylaxis, is medicine people at risk for HIV take to prevent getting HIV from sex or injection drug use.
In January 2021, the World Health Organization (WHO) recommended that the dapivirine vaginal ring (DPV-VR) may be offered as an additional prevention choice for women at substantial risk of HIV infection as part of combination prevention approaches.
Because Uganda largely depends on donor support for HIV/AIDS treatment and prevention, PrEP tools like the dapivirine vaginal ring (DPV-VR) and a twice-yearly injection known as lenacapavira are rolled out in a phased-funded approach, and therefore more women and adolescent girls continue to be infected despite the efficacy of these medications and tools.
A bio-behavioral survey conducted in 12 of Uganda’s regional towns found that 54 percent (over half of the sex workers aged 35-49 years) were living with HIV. The results of the survey released in October indicated that one in three commercial sex workers missed taking their ARVS at least once.
Dr. Geoffrey Musinguzi, the principal investigator, said each female sex worker had had a sexual encounter with at least four men. He suggested HIV pre-exposure prophylaxis (PrEP) could stop the majority of HIV transmissions that still happen in Uganda and most of the sub-Saharan countries.
Lynette Nangoma (not her real name) is one of the lucky female Ugandan women who have had the chance to have access to oral pre-exposure prophylaxis as well as the vaginal dapivirine vaginal ring. She told IPS that there are times when she forgets to take her PrEP pills. Nyangoma usually engages in multiple sexual relationships. ”Thank God I’m still alive and HIV-free. I think those tablets helped a lot. As you may know, this job of ours can be risky,” she narrates.
Dr. Daniel Byamukama, the head of HIV prevention at the Uganda Aids Commission, revealed that HIV prevalence remains high among key populations, at 33 percent among sex workers, 15 percent among prisoners, and 17 percent among people who inject and use drugs.
Nangoma told IPS that she has been using the dapivirine vaginal ring for the last four months.
“I feared it at first when a health worker was brought in to teach us about it. It looked too big. But I decided to try it. I can tell that for me, I find very convenient.”
The dapivirine vaginal ring is a female-initiated option to reduce the risk of HIV infection. It must be worn inside the vagina for 28 days, after which it should be replaced by a new ring. The ring works by releasing the antiretroviral drug dapivirine from the ring into the vagina slowly over 28 days.
Nangoma told IPS that some of her colleagues have been hesitant to use it, fearing discomfort.
Dr. Carolyne A. Akello, who has spent over 10 years in HIV/AIDS research with a focus on HIV prevention among women of reproductive age, including adolescent girls and young women, told IPS: “Yes, it looks big, but actually the vagina is a very accommodating organ. The ring is inserted into the vagina, and it is held up by the muscles. The ring was well researched. It is one size fits all. So whether small, big, or short, it fits every woman. It usually goes to the back of the vagina. There is where it sits for all the 28 days.”
“For a woman to use it consistently, we ask her to leave it there even during sex and menstrual periods. And many women, once they fix it, actually say, ‘Wow. The ring seems to have disappeared; I don’t feel it any more.’ And also, many men don’t feel it during sex. Seven out of ten men did not know that their partner was using the ring,” said Akello.
Unlike daily oral PrEP, dapivirine vaginal ring does not rely on remembering to take a pill each day and is also discreet as it stays inside the vagina throughout the month.
HIV/AIDS activist and access to medicine campaigner who leads the International Community of Women Living with HIV in Eastern Africa (ICWEA), Lillian Mworeko, told IPS that one of the advantages of the dapivirine vaginal ring is that it is discreet.
“It gives power to the woman in terms of control. They are able to fix it themselves. They are in charge. You are giving power to the woman to take care of their prevention. We strongly advocate for it,” Mworeko said. “So that women, especially adolescent girls and young women who are not able to negotiate for safer sex, have a tool that is in their control without seeking permission.”
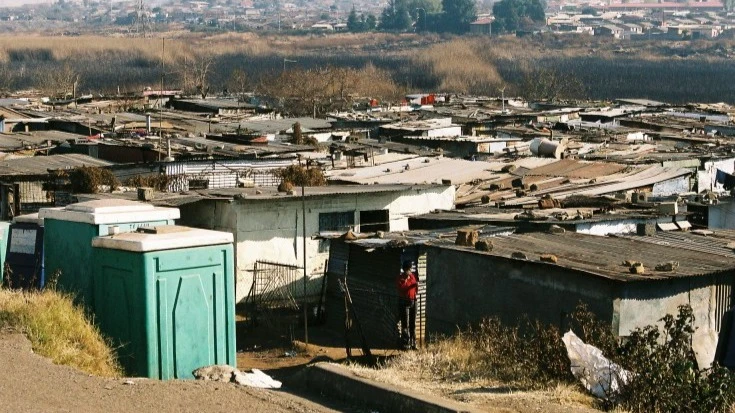
Uganda was among the first countries in sub-Saharan Africa to approve dapivirine ring. Others included Namibia, South Africa, Kenya, Zimbabwe, Zambia, Malawi, Rwanda, Eswatini, Lesotho, and Botswana. The ring was designed for women to use in countries that still carry a high level of stigma around HIV. In 2023, South Africa announced a national rollout of the ring. Eswatini, Zambia, Rwanda, and Kenya have embarked on similar efforts.
Dr. Diana Atwine, the Permanent Secretary at Uganda’s Ministry of Health, said the dapivirine vaginal ring is only available in seven districts funded by USAID under PEPFAR. Less than three hundred women had accessed the vaginal ring through that initiative by the end of August 2024.
While Atwine says lenacapavir will be a game-changer in terms of reducing the burden of daily pills and minimizing stigma and stigmatization, her ministry’s budget cannot afford the high cost of such tools.
As Uganda joins the rest of the world to mark World AIDS Day, Mworeko used the occasion to express her frustration that so many women in Africa cannot access these tools because their governments say they cannot afford them. Gilead Sciences, the company behind lenacapavir, reportedly charges the one-month ring, which currently costs USD 12.8 per month.
“When we talk about life and the lives of people, we need to put it into the context that nothing can compare with a person who is going to live with HIV for the rest of their life. We cannot compare the price of prevention with treating a person for life,” argues Mworeko.
She suggests that other than waiting for donations that delay or never arrive, the leaders of Africa must set part of their national budgets to ensure that women and girls have access to the new prevention tools and methods.
“What is the cost of preventing a young girl from getting HIV, and they are going to live the rest of their life free of HIV? They are going to deliver babies free of HIV, and they are going to contribute to the economy of their country. Compared to not acting now in the name of the cost, we are going to have this young person infected with HIV, and we must treat them,” Mworeko asked.
When asked about the facts that Uganda and other countries in Africa lacked money to make their own purchases of the prevention measures, Mworeko said, “What are our priorities? Who prioritizes what? We must prioritize where our hearts are. We cannot continue talking about new HIV infections when tools are here.”
Part of Mworeko’s frustration was partly directed towards researchers and the manufacturers of these medicines and preventive measures.
“I think the most disturbing situation is that most of the research is done here in our country. We are slow at rolling them out. Yet other countries pick up and fund these interventions. So we contribute to research, but we don’t benefit as a country. Because there is no one who would want to see their children infected with HIV,” says Mworeko, one of the activists behind the HIV Prevention Choice Manifesto for Women and Girls in Africa.
Uganda was among the countries where clinical trials for Gilead’s PURPOSE 1 were conducted. The results showed the high prevention effectiveness of the six-monthly long-acting injectable drug lenacapavir for cisgender adolescent girls and women, cisgender men, and transgender women.
The Global HIV Prevention Coalition (GPC), UNAIDS, and other partners called on Gilead Sciences to accelerate their efforts in ensuring that it is made available, accessible, and cost-effective, especially to low- and middle-income countries. It said the company’s approach must reflect the urgency of their needs.
“We urge Gilead to act swiftly in ensuring equitable, sustainable, broad access, particularly in markets with the highest need,” said GPC.
Gilead promised in early October that it will prioritize providing lenacapavir to Rwanda, South Africa, Tanzania, Thailand, Uganda, Vietnam, Zambia, and Zimbabwe until generic versions are available.
Dr. Flavia Matovu Kiweewa, one of the researchers on Gilead Sciences’ PURPOSE program in trials in Uganda, said: “I know Gilead Sciences has committed to providing licenses to generic manufacturers to make this product. But countries need to advocate so that we can be the first beneficiaries of lencapvir because we have significantly contributed to the study. But not only that, we are seeing lots of infections in young women.”
Dr. Herbert Kadama, the PrEP coordinator at the Ministry of Health, said Uganda plans to adopt lenacapvir and dapivirine vaginal ring are part of the efforts to address the challenges women also face with HIV/AIDS. He noted that 63 percent of new infections in Uganda, like the rest of Africa, are in women and girls.
According to Dr. Flavia Matovu Kiweewa, lencapvir prevents HIV acquisition by HIV-negative women by 100% compared to other preventive measures, but it is not a vaccine.
”We are glad that for the first time ever in history, we have an intervention that can give 100% protection against acquiring HIV. For us who have been in the PrEP field for quite some time, we faced lots of disappointments, especially for women trials. Because women are not able to adhere to daily interventions and they are influenced by their partners and friends,” said Matovu Kiweewa.
“Lenacapvir is going to be a game changer in the HIV prevention landscape. We are very excited that if we can access lanacapvir in Uganda and other high-burden settings in Africa, we will reduce the incidence of HIV significantly,” she added.
Top Headlines
© 2025 IPPMEDIA.COM. ALL RIGHTS RESERVED