A midwife in Gaza: Bringing life into the world during Israel’s war

NOUR Mwanis, a 27-year-old midwife, was still in the al-Awda Health Center delivery room with a woman who arrived early in the morning in labour.
The shift manager said she would need about half an hour to attend to the birth, clean up, and sterilise the room and equipment.
In the reception area, the grandmother, grandfather and uncles of a newborn were passing the baby around in a festive atmosphere.
Grandma beamed as she inspected the baby, swaddled in a pink scarf.
The happiness on their faces brought warmth and joy to hearts around them. This kind of happiness had been absent for a long time.
Asked about the baby girl’s name, they laughed gently and said: "She doesn’t have a name yet.”
A few minutes later, her mother was wheeled out on a gurney by two nurses who were taking her to the recovery area.
The department head said Nour was ready to meet, and she was, nearly.
Standing in the quiet delivery room, she looked up with a calm smile as she placed a tray of tools in the sterilizer, sanitised her hands, then sat on a bed to talk about being a midwife during a war.
Interrupting herself, Nour went out to reception to ask about labouring women and their progress.
The nurse at the desk said: “They’ll all need time. Until the second shift or tomorrow morning.”
"OK, we’ve got time to talk then," Nour said as she came back to sit on the bed.
Nour had dreamed of becoming a midwife, of helping women give birth safely and bringing joy to new families with smiles all around.
For three years, she had that. Then her dreams were devastated by the start of Israel’s war on Gaza in October.
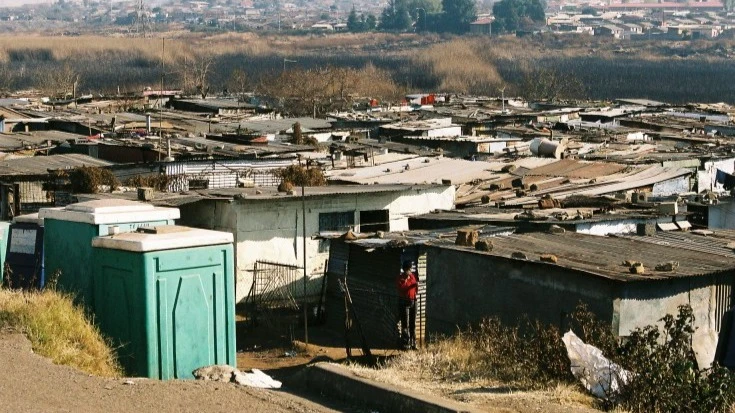
"I never expected to see days like these in my life," Nour told Al Jazeera of the massive influx of people who came to the Nuseirat refugee camp in central Gaza, trying to get away from Israel’s bombs by moving south.
"For the first three months of the war, we were handling about 60 to 70 births a day, working around the clock with just six midwives," she recalled.
She also was not able to go home for about three months. The pressure on the hospital and the perilous nature of moving around Nuseirat kept her in al-Awda.
"The delivery room couldn't accommodate the numbers. We had to assist some deliveries on the floor or in prenatal preparation rooms that weren’t equipped for childbirth," Nour explained.
The pressure on al-Awda grew after it became the only maternity facility in the Central Governorate after Al-Aqsa Martyrs Hospital in Deir el-Balah had to close its maternity ward to focus on treating the wounded.
"It was chaos - bombing all around, labouring women arriving in miserable conditions," Nour said with a deep sigh.
"Many women had complications, such as bleeding or stillbirths, and they needed special care.
“But it wasn't available, and they just got worse."
As if to prove her point, a nurse came in to tell Nour that 28-year-old Aya al-Kafarna had been admitted for a stillbirth.
Aya was 31 weeks pregnant, but her baby had died in the womb because she was so weakened by her displacement without access to enough food, clean water, medicine, supplements or medical care.
Aya’s father, a 58-year-old paramedic, had been killed in an Israel bombing, she said. One day later, she noticed that her baby had stopped moving in the womb.
Inducing labour was the only way to help Aya, Nour explained. Induced labour would extract a further emotional toll on Aya as well as a physical one because her body was not naturally ready to deliver.
"I was in complete shock, and I couldn’t stop crying at first," Aya said.
"But eventually, I tried to calm myself and reflect on the circumstances I’m living in.
"Maybe it’s for the best that this child doesn’t have to be born into such misery. Perhaps God has spared him from this suffering."
In December, the third month of the war, Nour was attending a delivery when she heard that her brother had been brought in, severely injured in an Israeli bombing.
"I nearly broke down because I hadn't seen my family for months and feared they were hiding the news of his death," she recalled.
"I ran through the hospital, screaming, until I reached him. He had severe injuries all over his body. I was crying uncontrollably."
But her brother was alive and eventually healed. He had been injured when the house next door was bombed, a strike that badly damaged the home they were sheltering in.
"Like all families, my family - my parents and nine siblings - was forced to move from one place to another during the war,” Nour said.
Throughout, she worked hard, wanting to be there for the labouring mothers, many of whom are brought to the hospital alone, weeping and in despair because they have lost loved ones.
"Women would be crying on the birthing bed, telling us about losing their children, husbands or families. This profoundly affects the birthing process," Nour explained.
"Psychological well-being is vital for the birthing mother. We'd try to offer some support. We’d embrace them or talk to them, try to comfort and reassure them.
"But there were so many cases that this wasn't always possible, especially in the early months."
Nour recalled one woman who went into labour on the day her husband was killed. In shock, she wept bitterly throughout the birth as she faced welcoming a new life into a world where her baby’s father had just been killed.
"It was an incredibly difficult situation, and we were at a loss for words to comfort her," Nour recalled, adding that the woman had trembled uncontrollably throughout, unable to regulate her emotions.
She had a baby boy whom she named after her husband and left the hospital fretting about how she would be able to provide for his needs.
An orderly rushed in, interrupting Nour, with a newborn in her arms who was struggling to breathe. Nour hurried over to help, ensuring the baby was stable and connected to oxygen.
Once the situation was under control, she returned, though she got up occasionally to check on the infant.
Births in which the mother had been injured in a bombing, sometimes having just been pulled from the rubble, were possibly even more heart-wrenching, Nour said.
"When the injury is to the back of a woman’s head, the birth becomes incredibly complex," Nour recalled. “We struggle to find a position for her to give birth safely.
"These situations … weren't in my training or the books we studied," Nour reflected.
"Childbirth isn’t a joyous welcoming of new life anymore," Nour reflected as she told the tales of women struggling to bring life into the world.
A woman eight months pregnant was brought in by neighbours and passers-by once, bleeding profusely from injuries she sustained while fleeing a bombing.
"The medical team tried hard to save her,” Nour said sadly, adding that the mother and baby did not survive.
She also witnessed five occasions when mothers were killed in bombings and doctors struggled to save the babies, succeeding only twice.
The tragedies Nour witnesses have taken a toll on her, and the early months of the war were exceptionally difficult because she lost touch with her family as she stayed on in the hospital.
"Sometimes communication would be cut off, and I’d be overwhelmed with anxiety whenever I heard about an attack anywhere," Nour said.
"All us midwives shared the same fears, so we tried to comfort one another.
"Some of us would break down with exhaustion and worry, and we’d take turns when someone needed a rest."
But being around births also reminds Nour that life goes on.
"War doesn’t stop life. People still have children. They still get married. It’s normal for people to continue living, even in abnormal circumstances."
“Even I got engaged during the war," Nour said, describing meeting a young volunteer with the hospital’s security team and falling in love.
She hopes the war ends soon so they can get married and start a new chapter of their life.
By Nour’s count, nearly all the labouring women who come to the hospital have severe inflammations that hinder safe deliveries.
"There's no clean food, clean water or hygiene supplies," Nour explained. "All these factors raise the risk of inflammations.
"Women come to deliver having not bathed for days, hair full of lice, and she’s coming to an unclean, unsterilised delivery area.”
The hospital staff managed to set aside a bathroom for women before they give birth, providing them with basic personal hygiene kits, including a razor, soap and shampoo, so they can wash.
But once they’ve given birth, they have to go back to their makeshift tents.
"Many women even beg us not to stitch their wounds after giving birth," Nour added. "They say: 'Please, I live in a tent with no bathroom. I don't want stitches.'"
Nearly all the displaced women have no access to clean water or to the gas to run a stove and boil water to sterilise it.
"Many women come back with infected stitches due to the poor living conditions,” Nour said.
It’s not just water that these new mothers lack. The sanitary pads they need after delivery are very hard to find and expensive if they are available.
"Women also say they can’t find privacy to breastfeed their babies because the tents are so overcrowded," Nour noted.
"We're talking about the bare minimum needs for a woman who has just given birth. They’re not available to women in Gaza."
The newborns of Gaza are not immune from what is happening to their mothers as birth weights decline by about 30 percent and their general health suffers.
"This reflects the malnutrition of pregnant women," Nour said.
There are also infectious diseases, such as hepatitis A, that are spreading in the overcrowded displacement camps and exacerbating the risks for pregnant women.
According to the Ministry of Health, 45,000 cases of hepatitis have been recorded during the war, a stark increase from just 85 cases the year before the war.
"We received several labouring women infected with hepatitis,” Nour said, explaining that infected women are at a higher risk for postpartum haemorrhaging.
"We had a woman with hepatitis. … We tried so hard to save her, but she died. We don’t have intensive care or an established protocol for cases like that," she added.
As the war goes on, the number of women in labour arriving at the hospital has decreased to about 15 a day.
“Palestinians are known for their love of family and children and how much they celebrate the arrival of births, but there are much fewer now,” Nour
concluded sadly.
By Maram Humaid
Top Headlines
© 2024 IPPMEDIA.COM. ALL RIGHTS RESERVED